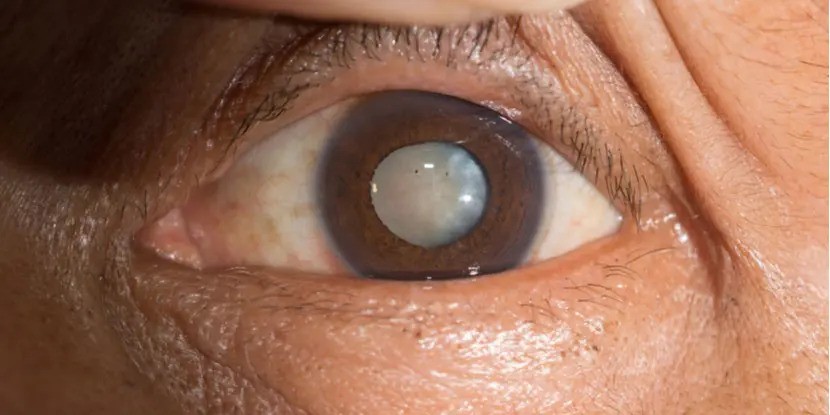
A cataract is a loss of transparency, or clouding, of the eye lens. The eye lens plays a vital role in focusing images on the retina. A cloudy lens interferes with light passing through to the retina, the light-sensing layer of cells at the back of the eye. Compare a cataract to looking at the world through a foggy or blurry window. Light rays do not focus clearly if the lens loses its clarity, as it does when a cataract develops. Glasses or contact lenses cannot sharpen vision if a cataract is present.

The most common cause of a cataract is aging. As you get older, chemical changes in your lens make it less transparent. The loss of transparency may be so mild that vision is hardly affected or so severe that no shapes or movements are seen, only light and dark. You have a cataract when the lens gets cloudy enough to obstruct vision to any significant degree.
Other causes of cataracts include trauma, medications like steroids, systemic diseases such as diabetes, and prolonged exposure to ultraviolet light. Occasionally, babies are born with a cataract. Glasses or contact lenses cannot sharpen your vision if a cataract is present.
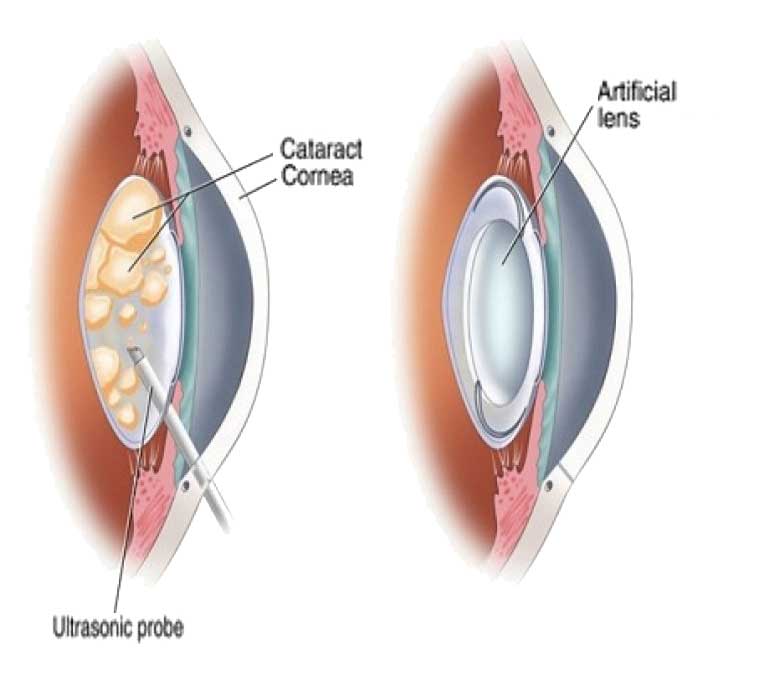
Reducing the amount of ultraviolet light exposure by wearing a wide-brim hat and sunglasses may reduce your risk for developing a cataract, but once set, there is no cure except to have the cataract surgically removed. Outpatient surgical procedures remove the cataract either through a small incision (phacoemulsification) or a large incision (extracapsular extraction). The time to have the surgical procedure is when your vision is bad enough to interfere with your lifestyle.
Cataract formation is a slow, progressive, and painless decrease in vision. Ironically as the lens gets harder, farsighted (hyperopic) people experience improved distance vision and are less dependent on glasses. However, nearsighted (myopic) people become more nearsighted, causing distance vision to worsen.
A cataract is detected during our comprehensive eye exams. Your eyes will be dilated, so the pupils are wide open, enabling our medical team to look for signs of a cataract with a slit lamp, along with checking your retina and optic nerve. We will also do a refraction to test your visual acuity.
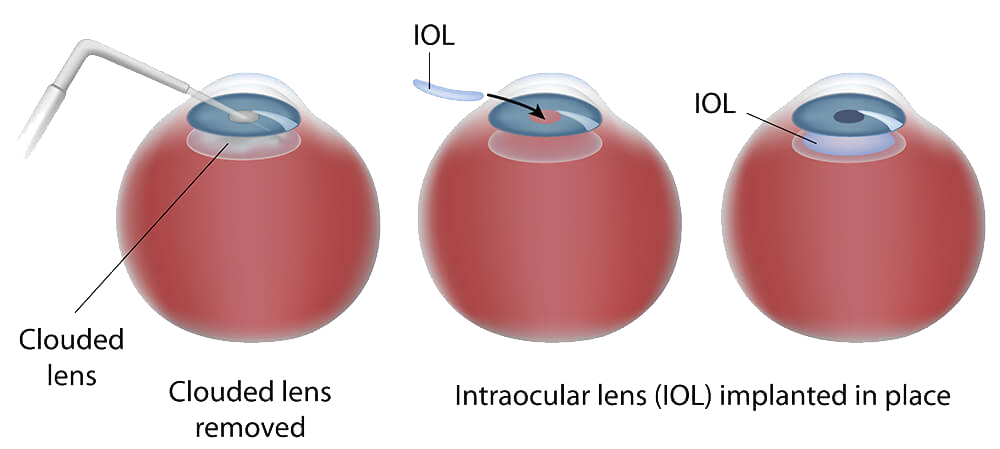
The treatment for a cataract is to remove the lens and implant an Intraocular Lens (IOL). An IOL is a tiny, lightweight, clear plastic disk placed in the eye during cataract surgery. Intraocular lenses have many advantages. The IOL remains in the eye after surgery, unlike contact lenses, which must be removed, cleaned, and reinserted. An IOL replaces the focusing power of the eye’s natural lens. The rapid evolution of IOL designs, materials, and implant techniques has made them a safe and practical way to restore normal vision after cataract surgery.
One and a half million people have a cataract procedure every year, and 95% achieve success. As with any surgery, complications may occur during or after, and some are severe enough to limit vision. In most cases, vision, as well as the quality of life, improves.
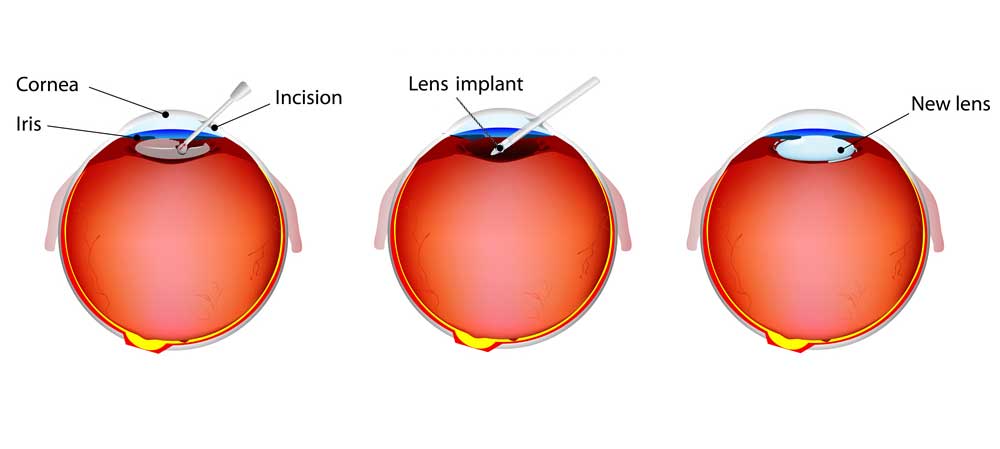
Laser-assisted cataract surgery is performed as an outpatient procedure, typically under a local anesthetic (using eye drops) or sometimes with general anesthesia. The patient feels no pain, but you may need to avoid bending over or lifting heavy objects during recovery. It can take up to six weeks to achieve the best-corrected vision.
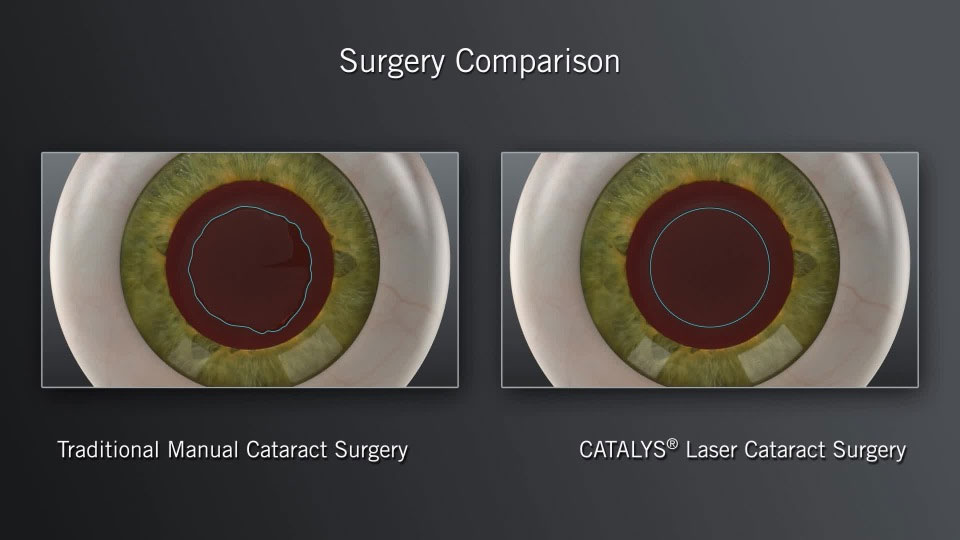
Femtosecond laser-assisted cataract surgery (FLACS) uses a computer-guided femtosecond laser to perform the most precise and demanding steps of traditional cataract surgery, including corneal incisions, the opening of the lens capsule (capsulotomy), and pre-softening the cataract for removal. This high-tech procedure offers potential benefits such as increased accuracy and reproducibility, precise astigmatism correction, and a reduction in the amount of ultrasound energy used during cataract removal.
Phacoemulsification is a surgical method in which an ultrasonic oscillating probe is inserted into the eye. The probe breaks up the center of the lens. The fragments are suctioned from the eye at the same time. A cataract is removed in tiny pieces with a small incision is made that does not require sutures to close. Most of the lens capsule is left behind, and a foldable intraocular lens implant, or IOL, is placed permanently inside to help focus light onto the retina. Vision returns quickly, and one can resume normal activities within a short period.
A posterior capsulotomy is a surgical laser procedure that is sometimes necessary after cataract surgery. It is painless and takes five minutes to perform.
During cataract surgery, part of the front (anterior) capsule that holds the lens is removed. The transparent back (posterior) capsule remains intact. As long as that capsule stays clear, one has good vision. But in up to 50% of people, the posterior capsule loses its clarity. When this happens, an opening can be made in the capsule with a laser (posterior capsulotomy) to restore normal vision.
Before the laser procedure, the ophthalmologist does a thorough ophthalmic examination to ensure there is no other reason for vision loss.
Cataract surgery has changed dramatically over the last 20 years. Many patients remember the days when the operation required a hospital stay of several days and weeks of recovery. Retinal detachment was a frequent complication and thick aphakic glasses were necessary for clear vision. Today’s cataract surgery is totally different. The operation is now done on an outpatient basis, usually only a two to three-hour stay.
New glasses, if necessary, are prescribed two to three weeks after surgery. If the second eye has a cataract it can be done within three to four weeks. Whether or not glasses are needed depends on the implant lens chosen.
Complications are rare and the success rate is in excess of 95%. The cataract will not grow back after surgery. However, the membrane, which supports the intraocular lens implant, can become cloudy in some patients months or years later. If this occurs, simple laser treatment is all that is necessary to restore clear vision.
It is helpful to consider vision from a lifestyle perspective. Considering what visual tasks are most important and if freedom from glasses for those tasks is important to you will help guide you on which IOL best matches your needs.
| Intraocular Lens | ||||
|---|---|---|---|---|
| Monofocal Standard | Toric Astigmatism | Extended depth of focus EDOF | Multifocal | |
| Customizable After Surgery | No | No | No | No |
| Astigmatism Correction | No | Yes | Yes | Yes |
| Zones of clear vision without glasses | Glasses likely needed at all distances for best vision | Distance | Distance, Intermediate | Distance, Intermediate, Near |
| Strengths | Most affordable | Excellent distance vision without glasses | Excellent distance and intermediate vision | Excellent full range of vision (distance, intermediate, & near) |
| Weaknesses | Glasses likely needed at all distances for best vision | Glasses required for intermediate and near tasks | May need glasses for near tasks and low light (within 20 inches) | Halos given lens design including low risk of glare |
| Optimal patient | Doesn't mind wearing glasses or can't afford other options | Prioritizes distance activities, ok with glasses for computer and reading | Fits with modern lifestyle, ok with glasses for reading and low light | Needs full range of vision, ok with low risk of bothersome halos |
| Good choice with coexistent ocular disease | Yes | Yes | Probably | No |