
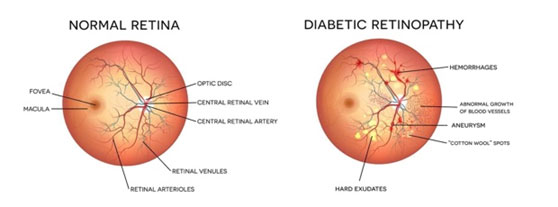
Patients with diabetes may develop diabetic retinopathy (when the tiny blood vessels in your retina weaken). This is when high blood sugar levels cause damage to blood vessels in the retina. These blood vessels can swell and leak. Or they can close, stopping blood from passing through. Sometimes abnormal, new blood vessels grow on the retina. All of these changes can steal your vision.
There are two main types of diabetic retinopathy.
Nonproliferative retinopathy (NPDR) is when your retina blood vessels leak and then close. In the early stages, there are few symptoms, but as it progresses, fluid deposits and swelling can cause moderate to severe vision loss.
Proliferative diabetic retinopathy (PDR) happens when the retinal blood vessels are so damaged that they close off. In response, the retina grows new, fragile blood vessels. Unfortunately, these new blood vessels are abnormal. They multiply on the retina’s surface and do not resupply it with blood.
Occasionally, these new blood vessels leak and cause a vitreous hemorrhage. Blood in the vitreous, the clear gel-like substance that fills the inside of the eye, blocks light rays from reaching the retina. A small amount of blood will cause dark floaters, while a significant hemorrhage might block all vision, leaving only light and dark perception. The new blood vessels can also cause scar tissue to grow. The scar tissue shrinks, wrinkling and pulling on the retina and distorting vision. The macula may detach from its normal position and cause vision loss if the pulling is severe.
You can have diabetic retinopathy and not know it. This is because it often has no symptoms in its early stages. As diabetic retinopathy gets worse, you will notice symptoms such as:
Diabetic retinopathy symptoms usually affect both eyes.
Diabetic retinopathy develops slowly, often with no early warning signs. If you have diabetes, you should be seen by your Ophthalmologist regularly and have a dilated eye exam at least once a year. Keeping your blood sugar, blood pressure, and cholesterol under control is essential. In later stages of the disease, injections or surgery may be required to treat it.
The screening exam consists of a complete, dilated examination of the eye and retina. The amount of diabetic retinopathy and risk for vision loss is assessed by carefully looking at the retina. If any complications are present, they can be detected and properly treated. Optical Coherence Tomography (OCT) is a retina scan, often performed to examine the retinal structure. OCT is beneficial for assessing macular edema. The measurement follows the response to treatment. Sometimes a Fluorescein Angiogram (FA) is performed. This test uses a special dye to check the blood flow in the retina and identify areas of leakage.
Treatments include intravitreal injections and laser surgery to shrink the abnormal blood vessels and reduce the risk of bleeding. A vitrectomy is performed if a vitreous hemorrhage is not cleared up or a retinal detachment is detected.